SOAP Notes Overview
SOAP Notes Overview
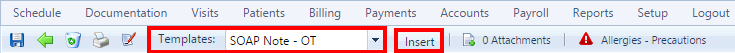
The SOAP section of the Visit screen is where you add the notes about a patient's session, The notes are required by insurance providers. SOAP stands for:
- Subjective
- Objective
- Assessment
- Plan
The notes table is divided into sections based on the acronym.The top part of the screen displays information about the patient and the visit. The information from the Treatments section of the Visit screen is populated with the CPT Code, Unit, and so on. A free form text field is available to add note.
The Objective and Assessment sections are populated from the Plan of Care with short and long term goals. You can rearrange the items in the list by changing the number or remove the check mark to delete the goal from the list. If you edit the notes, the goal still appears and you can click the check box to add it back to the goals. Complete the notes as required. A free form text field also appears below the goals for you to add other notes.
The Plan section is a free form text field where you can add more care plan information.

Created with the Personal Edition of HelpNDoc: Create cross-platform Qt Help files