Documentation Overview
Documentation
Overview
The Documentation portion of the application is where all of the documentation is stored, edited, or created. Diagnosis codes are also stored with the documentation in the Evaluation. The types of documentation you can create include:
 Create a new or re-Evaluation
Create a new or re-Evaluation  Create a new CarePlan
Create a new CarePlan  Create a new Summary/DC (Discharge) Summary - There must be at least one visit
Create a new Summary/DC (Discharge) Summary - There must be at least one visit Create a new Progress Note (Daily Note) (visit must already exist)
Create a new Progress Note (Daily Note) (visit must already exist) Create a new Patient Form
Create a new Patient Form Copy existing/signed Evaluations and CarePlans
Copy existing/signed Evaluations and CarePlans Print selected documents from the chart (prints to PDF by default)
Print selected documents from the chart (prints to PDF by default) Email/Fax/Dispatch selected documents from the chart (currently unable to dispatch Summary)
Email/Fax/Dispatch selected documents from the chart (currently unable to dispatch Summary)
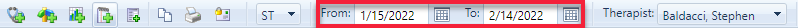
You can filter a patient's documentation list by date range
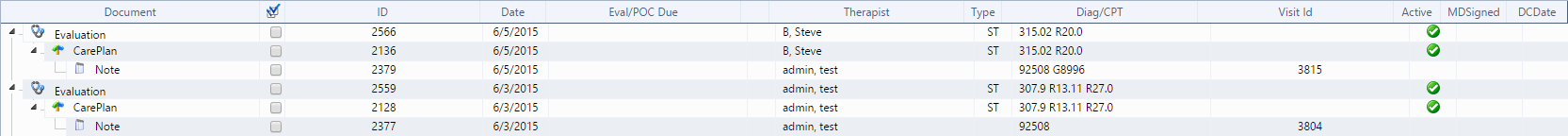
Before you can create new documentation or edit documentation, you must select a therapist from the drop-down list on the toolbar then select a patient. A list of that patient's documentation appears and includes:
- Patient Forms
- Evaluations or Re-evaluations
- Care Plans
- New Summary/DC Summary
- Progress Note
IMPORTANT: Only the person who creates the documentation can sign the documentation unless a non therapist creates the document (Admin). In other words, the document will be owned by the person who is logged into ClinicSource and creates the documentation. If you create documentation with a therapist's name other than yourself, that therapist cannot sign the documentation, only you can sign unless a non therapist creates the document (Admin).
You can copy documentation, edit documentation, and delete items in tables. After making your changes, electronically sign the document.
Created with the Personal Edition of HelpNDoc: Full-featured Help generator