Sign SOAP Notes
Sign SOAP Notes
When the visit is complete the, the notes must be signed by the therapist and by the supervising therapist. Before the supervisor can sign the notes, the therapist must sign them. Signed visits are indicated by pen buttons in the Visit window.
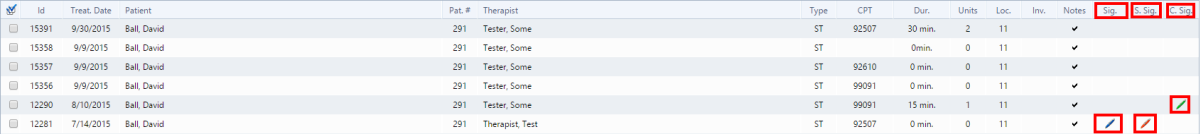
- Blue pen button indicates the therapist signed the note.
- Red pen button indicates the supervisor signed the note.
- Green pen button indicates the patient/caregiver signed the visit.
Therapist Signature
Follow these instructions to sign the SOAP notes:
1.In the Visits window, Patients section, select the patient you need. The patient's visits list appears.
2.From the patient's list, select the visit you want to sign. The Visit window appears.
3.In the header of the visit, click the Edit  button . The Notes table is editable.
button . The Notes table is editable.
4.Click the pen button in the visits tool-bar. The signature appears in the appropriate area below the notes.
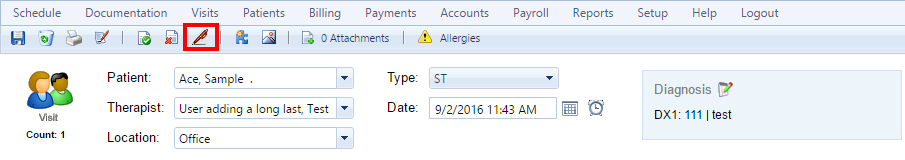
5.Click the Save  button to save the signature.
button to save the signature.
Supervisor Signature
Follow these instructions to sign the SOAP notes:
1.In the Visits window, Patients section, select the patient you need. The patient's visits list appears.
2.From the patient's list, select the visit you want to sign. The Visit window appears.
3.In the notes section, click the Edit  button The Notes table is editable.
button The Notes table is editable.
4.Click the pen button in the notes tool-bar. The signature appears in the appropriate areas below the notes. Note that the pen has a small letter S above it indicating that the supervisor only can sign the notes .
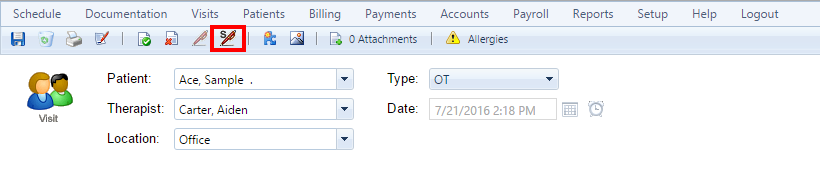
5.Click the Save  button to save the signature.
button to save the signature.
Created with the Personal Edition of HelpNDoc: Eliminate the Struggles of Documentation with a Help Authoring Tool